Espacios. Vol. 36 (Nº 11) Año 2015. Pág. 3
Impact of changes in meteorological and hospitalizations for asthma
Impacto das mudanças na meteorologia e hospitalizações por asma
Amaury de SOUZA 1; Débora A. da Silva SANTOS 2; Ana Paola de Souza LIMA 2; Flavio ARISTONE 1
Recibido: 15/02/15 • Aprobado: 24/04/2015
Contenido
ABSTRACT: |
RESUMO: |
1. Introduction
Environmental factors affect the dynamics of asthma, increasing its severity and morbidity rates. What is noticeable among these factors is the presence of air pollutants (both indoor and outdoor) and the meteorological conditions of the places, including temperature, relative humidity and wind speed, which may increase the duration of exposure to pollutants, as well as preventing pollutants from dissipating.[1,2]( Nishima S, et al, (2009); Braman SS. (2006)
Among the climatic variables, wind speed and relative humidity (when interacting with air pollution) have been correlated with an increase in the incidence of asthma exacerbations. In corroboration of this fact, a study describing the distribution of asthma attacks in relation to local meteorological factors (temperature, relative humidity and rainfall) revealed that relative humidity was correlated with bronchial asthma in adults.[3,4]( Suissa S, Ernst P. (2003); Bateman ED et al, (2008)
Both weather [5–8] (de Diego Damia A et al, 1999; Abe T et al , 2009; Ho WC et al, 2007; Lipsett M, Hurley S, Ostro B. ,1997) and air pollutants [7–13] (Ho WC et al, 2007; Lipsett M, Hurley S, Ostro B. ,1997; Barnett AG et al, 2005; Villeneuve PJ, Chen L, Rowe BH, Coates F. 2007; Stieb DM, et al, 1996; Tecer LH et al, 2008; Yamazaki S, Shima M, Ando M, Nitta H. 2009) have been recognized as important environmental factors that have adverse effects on asthma. Most of these factors have been the focus of extensive research, but there is a number of environmental factors that have not yet been fully evaluated in terms of their effect on asthma.
First, it has recently been suggested that temperature fluctuation rather than ambient temperature itself is related to cardiovascular disease [14, 15] (Cao J, 2009;. Kyobutungi C, 2005) However, we are unaware of studies which have evaluated the effect of temperature fluctuation on the exacerbation of asthma. One of the hypotheses of this study is that fluctuations in ambient temperature could increase the risk of asthma hospitalization; consequently, we have examined the association between temperature fluctuation and asthma hospitalization.
Second, it is necessary to evaluate the health effects of air pollutants. Air pollutants have also been emphasized as important triggers of asthma exacerbation [7–13] (Ho WC et al, 2007; Lipsett M, Hurley S, Ostro B. ,1997; Barnett AG et al, 2005; Villeneuve PJ, Chen L, Rowe BH, Coates F. 2007; Stieb DM, et al, 1996; Tecer LH et al, 2008; Yamazaki S, Shima M, Ando M, Nitta H. 2009), and several studies have reported an effect after a lag of a few days following exposure [8, 10–12] (Lipsett M, Hurley S, Ostro B.,1997;Barnett AG et al, 2005; Villeneuve PJ, Chen L, Rowe BH, Coates F. 2007; Stieb DM, et al, 1996). In Japan, there have been a few studies which evaluated the short-term effect of air pollutants on asthma exacerbation, but these focused on the effect on asthma of exposure on the same day and on the previous day [6, 13] (Ho WC et al, 2007; Yamazaki S, et al, 2009). In this study, we evaluated the lagged effect of air pollutants for up to 6 days prior to hospitalization.
The study was conducted in the municipality of Campo Grande, considered medium size, with intense activity of fires. This municipality is located in the Brazilian Midwest, with a population of approximately 724,000 inhabitants spread over an area of 8,096 km2, and high degree of economic development, highlighting the importance of agribusinesses.
Therefore, the overall aim of this study was comprehensively examine the effects of fluctuations in ambient temperature, ozone, and AD events in the city of Campo Grande on the exacerbation of asthma in children using hospital data.
2. Materials and methods
Data Collection
The city of Campo Grande - MS, (20° 27'16 "S, 54° 47'16" W, 650 m), is located on the plateau called Maracajú-Campo Grande, 150 miles from the start of the largest floodplain in the world, the Pantanal (139 111 km2), and an estimated population of 724,000 inhabitants. Souza et al, 2009 [16]; using the Koppen's method, the climate in the region of Campo Grande, is the type with moderate temperatures ranging from 17.8 °C minimum, 29.8 °C maximum and average of 22.7 °C, with hot summer and well distributed rainfall, average relative humidity is 72.8%.
Souza & Granja (1997) [17] found prevailing winds in East Campo Grande - MS, occurring in the North in months from January to December, with annual values resulted in 24% of East, 19.8% of North and 12,2% of Northeast, and the lulls represented 12% with an average speed of 3.1 m/s, and average monthly rainfall in 122,4mm and annual average 1469 mm.
For the correlation of weather data with the aggravation of respiratory illnesses, hospitalization data were collected from the health agencies of SUS (Unified Health System ) and Department of Informatics (DATASUL).
The available data came from the Hospital Information System of SUS (SIH / SUS), managed by the Ministry of Health, through the Department in Health Care, in conjunction with the State Departments of Health and the Municipal Health and processed by Datasus at the Executive Department of the Ministry of Health.
All hospitalizations occurred in the period between January 1st, 2008 and December 31st, 2010, the diseases investigated were coded according to the International Classification of Diseases (CID) 10th Revision, asthma (J45). The subjects of this study were children under 9 years of age.
Information about daily levels of ozone (O3) were obtained from the Institute of Physics of UFMS. The Ozone Analyzer, used for the measurements has as working principle the absorption of ultraviolet radiation by the ozone molecule. These measurements are performed continuously 24 hours a day; every 15 minutes are provided values of the ozone concentration. The analyzer is installed near Campo Grande, away from local sources.
Data Analysis
We controlled for seasonality and long-term trend using a natural cubic spline with 7 df per year for time. To control any confounding weekly pattern, the day of week was also included as an indicator in our analysis. Public holiday was controlled as a binary variable. We also controlled for relative humidity. We evaluated the model fit using Akaike's Information Criterion for quasi-Poisson (Q-AIC). The results showed that models that controlled humidity had lower Q-AIC values, indicating that models including humidity were a better fit (results not shown). We used mean temperature to assess temperature effects in this analysis since itwas found to be a better predictor (i.e. had lower Q-AIC values) than the maximum and minimum temperatures. We used a DLNM with 5 degrees of freedom natural cubic for temperature(knots at equally-spaced percentiles by default) andwith 4 degrees of freedom natural cubic for lags (knots at equally-spaced values in the log scale of lags by default) (18). The median value of the mean temperature (23.6 °C) was used as the reference value (centering value) to calculate the relative risks. A maximum lag of 30 was used to completely capture the overall temperature effect and adjust for a possible harvesting effect (18). We examined and plotted cumulative relative risks with temperaturefor lag 0, ....... and 0–30.
3. Results
Daily hospital admissions, environmental data and air pollutants from January 1, 2008, to December 31, 2010, are shown in Table 1. During this time period, totaling (1094 days) 5,844 hospital admissions for asthma were recorded in Campo Grande, a mean of 5.3 hospitalar admissions per day (range, 2–13). Admissions varied seasonally, with the peak number in winter, followed by autumn. During the study period, the DMT was 23.6°C (range, 7.0–30.6°C). The mean relative humidity (RH) was 66.6% (range, 21.9–79.1%), the mean rainfall was 3.9 mm (range, 0–111.0 mm/day) and the mean wind speed (WS) was 3.0 m/s (range, 0.4–10.5 m/s). Mean concentration of ozone (o3) was 17.1 ppb (range, 2.0- 29.3 ppb).
Table 1- Summary statistics of daily asthma admissions, meteorological factors and air pollutants over 1094 days.
Variable |
Total Count |
Mean |
SDa |
Minimum |
p(25) |
Median |
p(75) |
Maximum |
ASTHMA |
1094 |
5.3 |
1.9 |
2.0 |
4.0 |
5.0 |
6.0 |
13.0 |
DMT(°C) |
1094 |
23.6 |
3.5 |
7.0 |
22.1 |
24.1 |
25.7 |
30.6 |
DHT(°C) |
1094 |
29.9 |
3.8 |
10.9 |
28.4 |
30.7 |
32.4 |
38,3 |
DLT(°C) |
1094 |
18.8 |
3.5 |
4.3 |
17.1 |
19.7 |
21.3 |
26,7 |
RHM(%) |
1094 |
66.6 |
15.6 |
21.9 |
55.5 |
69.1 |
79.1 |
97.7 |
RHM(%) |
1094 |
82.7 |
14.6 |
30.0 |
76.0 |
88.0 |
94.0 |
98 |
RHL (%) |
1094 |
44.8 |
17.5 |
11.0 |
31.0 |
43.0 |
55.0 |
97 |
WS Km/h |
1094 |
21.2 |
5.8 |
8.6 |
16.8 |
20.5 |
24.5 |
43.6 |
JS(mm) |
1094 |
3.9 |
10.2 |
0.0 |
0.0 |
0.0 |
1.6 |
111.0 |
| O3(ug/m3) | 1094 |
17.1 |
3.6 |
2.0 |
14.7 |
16.6 |
19.3 |
29.3 |
DMT: daily mean temperature; DLT: daily lowest temperature; DHT: daily highest temperature; RHM daily mean relative humidity; RHH daily highest relative humidity: RHL: daily lowest relative humidity JS: rainfall; WS: wind speed. aStandard deviation.
Hospital admissions for asthma and daily temperature over time are presented in Figure 1. Hospital admissions varied seasonally. DMT showed significant periodicity, as well as random fluctuations. However when DMT was relatively low, the number of asthma hospital admissions appeared higher.
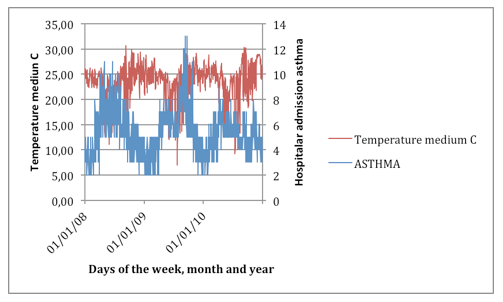
Figure 1-Daily mean temperature and daily hospital admissions
for asthma over time in Campo Grande, Brazil during 2008 to 2010.
----
Table 2-Pearson's correlations among asthma hospital admissions, meteorological factors and ozone.
|
ASTHMA |
DMT(°C) |
DHT(°C) |
DLT(°C) |
RHM(%) |
RHM(%) |
RHL (%) |
WS Km/h |
JS(mm) |
DMT(°C) |
-0,214 |
||||||||
DHT(°C) |
-0,151 |
0,917 |
|||||||
DLT(°C) |
-0,306 |
0,891 |
0,696 |
||||||
RHM(%) |
-0,213 |
-0,353 |
-0,521 |
-0,017 |
|||||
RHM(%) |
-0,201 |
-0,196 |
-0,312 |
0,013 |
0,808 |
||||
RHL (%) |
-0,128 |
-0,369 |
-0,577 |
-0,047 |
0,846 |
0,425 |
|||
WS Km/h |
0,109 |
-0,066 |
-0,016 |
-0,069 |
-0,229 |
-0,222 |
-0,172 |
||
JS(mm) |
-0,135 |
-0,1 |
-0,192 |
0,064 |
0,401 |
0,303 |
0,367 |
0,09 |
|
O3(ug/m3) |
0,001 |
0,215 |
0,263 |
0,122 |
-0,378 |
-0,385 |
-0,25 |
0,224 |
0,001 |
Pearson's correlations between daily hospital admissions for asthma, meteorological factors and ozone are shown in Table 2. Daily hospital admissions showed significant negative correlations with DMT (r=−0.214, P<0.001), rainfall (r=−0.135, P<0.05) and WS (r=−0.043, P<0.05). Daily hospital admissions for asthma showed significant positive correlations with O3(r=0.001, P<0.05). DMT showed significant negative correlations with relative humidity (r=-0.213, P<0.001), rainfall (r=-0.100, P<0.001) and WS (r=0.099, P<0.001)). Relative humidity showed a significant positive correlation with rainfall (r=0.401, P<0.001), and reversely, significant negative correlations with O3 (r=−0.378, P<0.001).
The cumulative effects of DMT on hospital admissions for asthma, including lag times, at the 25th and75th percentiles of temperature relative to the median temperature are depicted in Table 3. When estimating the cumulative effects of cold temperature on asthma admissions, we found that cold temperature significantly increased the risks of hospital admissions at lag times of 14 to 30 days. For example, the relative risk of asthma hospital admissions associated with the 25th percentile of temperature relative to the median temperature was 1.20 (95% confidence interval [CI], 1.01~1.41) at lag 0–14. However, the association between high temperatures (the 75th percentile of temperature relative to the median temperature) and asthma hospital admissions is limited (RR= 0.90, 95% confidence interval [CI], 0.80~1.01)).
Table 3- Relative risk of asthma admissions associated with change in DMT between selected cutoff points.
Lag effects |
25th percentile relative to |
75th percentile relative to |
0 |
1.03(0.95,1.12) |
1.00(0.95,1.06) |
0–1 |
1.03(0.94,1.11) |
1.02(0.96,1.08) |
0–2 |
1.04(0.94,1.15) |
1.01(0.94,1.08 |
0–3 |
1.01(0.91,1.13) |
1.03(0.95,1.10) |
0–7 |
1.09(0.95,1.26) |
0.98(0.89,1.07) |
0–14 |
1.20(1.01,1.41) |
0.90(0.80,1.01) |
0–21 |
1.28(1.04,1.58) |
0.83(0.71,0.97) |
0–30 |
1.48(1.14,1.92) |
0.75(0.62,0.91) |
4. Discussion
In Brazil, asthma hospitalization rates vary according to the locale studied and the regional environmental characteristics. The frequency of hospitalization found in the Emergency Room of Hospital do Servidor Público de São Paulo (São Paulo Hospital for Public Employees) was 1.8%. In 1996, most such hospitalizations occurred in hospitals located in rural areas of Brazil and operating under the Unified Health System. That year, asthma was the fifth leading cause of hospitalization nationwide (excluding childbirth and puerperal disorders), the third in the northeast, the fourth in the north and south, and also the fifth in the central-west and southeast regions (Chatkin JM et al, 1986).[19]
Other Brazilian studies have shown the significance of asthma as a cause of hospitalization. From July of 1983 to June of 1994, asthma was responsible for approximately 18.6% of all hospitalizations due to acute respiratory diseases among children under five years of age at all pediatric hospitals in the city of Porto Alegre, located in the state of Rio Grande do Sul (Trippia SMG, Rosário Filho N, Ferrari FP. ,1998 )[20]. In the city of Santo André (in the state of São Paulo), asthma attack was found to be one of the three leading causes of hospitalization among children treated in the emergency room. In various locations, hospitalization due to asthma occurred more often among children under five years of age, especially in those under two years of age. Asthmatic children presenting more severe clinical profiles tend to have recurring attacks and, consequently, present multiple hospitalizations.
The influence of environmental variables on the triggering of asthma attacks has been described by several authors. In a study of asthmatic children up to fourteen years of age, the main precipitating factors found to be potentially correlated with attacks were changes in climate (in 78% of the children studied), upper airway infections (in 65%) and exposure to house dust (in 52%)[21] (Fischer G B. 1984). In another study, climatic influences (temperature and relative humidity) were also correlated with the incidence of asthma attacks [22] (Guirau LM, Solé D, Naspitz CK. ,1997). In one study, climatic changes were found to be the main triggering agents of asthma attacks and upper airway infections in the first year of the disease, regardlessgender (Pastorino AC et, 1998 ).[23]
The influence of climatic changes, particularly sudden drops in temperature, has been found to be potentially correlated with greater dispersion of aeroallergens, leading to a higher frequency of asthma attacks.[24-26] (Fiore RW et al , 2001; Correia AL et al, 2001; Pastorino AC, et al, 1998) . As previously mentioned, the climate in the city of Campo Grande is divided into a dry season (from May to October) and a wet season (from November to April). The hypothesis of the present study is that, in the dry season, through the influence of low relative humidity and high temperatures, asthma control is affected due to an intensification of the attacks and of their severity (Martinez FD et al, 1995).[27]
The frequency of hospitalizations due to asthma attacks was higher in the months of April, May and June, just the final period of the rainy season and beginning of the dry season. In these months, the rate was two to three times higher than in the rainy season. It is possible that most of asthma treatment rate found in the rainy season is correlated with excessive moisture due to heavy rains and constant, the places frequented by children, and that this could cause diseases ranging from the common cold to a frame more severe acute respiratory infection, which are risk factors for asthma and confounding factors in triggering diagnosis. In addition, children spend most of their time at home and in contact with all the allergens present in the domestic environment, which are more numerous in this period due to the higher growth of fungi caused by excessive moisture (Zhang L et al, 1999). [28]
To our knowledge, this study is the first to assess the effects of DMT on hospital admissions for asthma in Campo Grande, over a 3-year period. We observed a statistically significant relationship between DMT and hospital admissions for asthma. Asthma hospital admissions varied seasonally, peaking in winter. The DMT effect increased significantly below the median temperature, consistent with previous findings (Tecer LH et al, 2008) [12]. In our analysis, we found a 48% increase in asthma hospitalization with the 25th percentile of temperature relative to the median temperature at lag 0–30. These results are consistent with a study conducted in eight cities in Koreas that found a significance in the association between asthma hospitalization and low temperature, with 43.6% increased at lag 0–32 (Son J-Y, Bell ML, Lee J-T, 2014) [29]. In Shanghai, Guo et al, 2012.[30] confirmed the association between asthma in children and cold temperature. Cold temperature, which was related to exacerbation of respiratory diseases, has often been followed by an increase in bacterial and viral infections of the airways, infiltration of inflammatory factors, and mucus secretion (Lipsett M, Hurley S, Ostro B. 1997), Donaldson G et al, 1999) (Larsson K et al, 1988) ([8], [31], [32]. Cold temperature has been associated with increased in the incidence of respiratory tract infections, and reduced temperatures often precedes the onset of infections , findings that may explain, at least in part, the effects of DMT on asthma.
We also observed that low temperatures had extended effects on hospital admissions for asthma, with lag periods of 14 through 30 lag days. The cold effect appeared to be relatively acute, lasting for several weeks. Although the relationship between DMT and asthma admissions had not previously been evaluated, several previous studies found that hot and cold temperatures has significant impacts on morbity/mortality rates in Campo Grande. Moreover, there is a delay between changes in daily temperature and changes in the incidence and mortality from diseases, although the lag periods varied in different studies. Higher temperature were found to have short term effects on mortality and morbidity (Mäkinen TM et al, 2009; Basu R, Samet JM, 2002) [33], [34], whereas the effects of low temperature were delayed and lasted for several days (Hajat S, Haines A 2002) [35]. An analysis in south China reported that hot temperatures had an acute but short-term effect, whereas the effect of dry station/cold temperatures lasted 10–12 days (Goodman PG, Dockery DW, Clancy L, 2004) [36]. Similar findings were observed in Chiang Mai City, Thailand (Yang J et al, 2012)[37]. However, we failed to identify significance in the association between hot period and asthma hospital admissions. Some previous results reported the similar effects (Guo Y, Punnasiri K, Tong S 2012) [38][. While the cold effects from ambient temperature are clear, that of hotter temperature appears inconsistent. Because temperature affects many asthma risk factors that vary in prevalence and seasonality by region, patterns of association between temperature and asthma are also expected to differ geographically (Xu Z et al, 2013)[39]. The magnitude and direction of the effects of temperature on asthma hospital admissions may be related to differences in the levels of exposure, susceptibility of subpopulations, public health interventions, health and social care services, and physical acclimatization (Buckley JP, Richardson DB 2012; Anderson GB, Bell ML, 2011) [40], [41].
This finding suggests that a longer time frame is required to capture the effects of cold, and that it may be inappropriate to specify an identical time frame for exposure to cold and hot temperatures. We investigated the effects of temperature on hospital admissions for asthma using a sophisticated statistical approach. As the dose-response curve relating these two factors is not exactly linear below and above a threshold, it is inappropriate to use linear threshold models to directly estimate these effects. DLNMs, which unify many previous methods in one unique framework, are flexible enough to describe non-linear dependencies and delayed effects of exposure at the same time (Michelozzi P et al, 2006)[42]. DLNMs can be easily translated into other study designs and regression models (Gasparrini A, Armstrong B, Kenward M, 2010) [43]. In the present study, we fitted DLNMs to fully understand the dose-response function and lag effects of temperature.
This study had several limitations. Firstly, we use weather conditions at one meteorological station as measurements of DMT rather than measures of personal exposure. The use of ambient rather than personal exposure measures may result in exposure misclassification. Moreover, the temperature difference between indoors and outdoors due to air conditioning or heating may affect the association between temperature and asthma. Secondly, the data on asthma hospital admissions were collected from Unified Health System, in Campo Grande, thus possibly introducing a selection bias. Thirdly, daily mean concentrations of ozone may vary more than daily mean temperature, which leads to limited ability to account for local differences in air pollutants with respect to asthma hospital admissions. This might reduce the power of the study, but it is not likely to attenuate the risk estimates. Finally, although the occurrence of asthma has been reported to be closely related to age and gender (Gasparrini A , 2011; Almqvist C, Worm M, Leynaert Bnd , 2008; Xu Z et al, 2013) [44], [45], [46], this study did not use the models for subgroup analysis.
The use of secondary data collected from health facility (emergency room) medical charts may have caused some biases. Therefore, some comments regarding the method are pertinent. First, we must consider the lack of some data that could have facilitated the analysis of the study variables, as is the case for health records compiled for other purposes. Data regarding family history of asthma or atopic, passive smoking and the nutritional state of the children, among others, were not available. This makes it difficult to understand the process as a whole since it limits the depth of the analysis of the results found, making it impossible to create study outlines in order to also measure the individual exposure of the child to the risk factors for asthma attacks.
We must consider the quality of the data registered regarding the definitive diagnosis made after the clinical examination of the child in the emergency room. It is known that the margin of error increases significantly due to the type of work that the pediatrician of the emergency room faces since the demand is considerable and the job is tiring. This leads to the allocation of less time for each child, thereby favoring the occurrence of misinterpretations of the signs and symptoms presented by the child.
5. Conclusions
This study demonstrated that hospital admissions for asthma were significantly associated with DMT below the median temperature. The effects of low temperature on hospital admissions showed a lag effect, lasting from 14 days to 30 days. The cold effect appeared to be relatively acute and lasted for several weeks. The findings suggest that cold temperature may trigger asthma attacks and that effective strategies are needed to protect populations at risk from the effects of cold. It was clear that children under nine years of age are more predisposed to the complications of the asthma attacks, more often requiring hospitalization, in the dry season.
Acknowledgement
We would like to extend our gratitude to the many people who helped to bring this article to fruition. First of all the UFMT. Ana Paola de Souza Lima for the contribution in English reviewing.
References
1-Nishima S, Chisaka H, Fujiwara T, Furusho K, Hayashi S, et al. (2009). Surveys on the prevalence of pediatric bronchial asthma in Japan: A comparison between the 1982, 1992, and 2002 surveys conducted in the same region using the same methodology. Allergology International 58: 37–53.
2=Braman SS. 2006. The global burden of asthma. Chest.130:4S–12S.
3-Suissa S, Ernst P. 2003. Use of anti-inflammatory therapy and asthma mortality in Japan. Eur Respir J. 21:101–4.
4-Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ. 2008. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 31:143–78.
5-de Diego Damia A, Leon Fabregas M, Perpina Tordera M, Compte Torrero L. 1999. Effects of air pollution and weather conditions on asthma exacerbation. Respiration. 66:52–8.
6-Abe T, Tokuda Y, Ohde S, Ishimatsu S, Nakamura T, Birrer RB. 2009.The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emerg Med. 27:153–9.
7-Ho WC, Hartley WR, Myers L, Lin MH, Lin YS, Lien CH, Lin RS. 2007. Air pollution, weather, and associated risk factors related to asthma prevalence and attack rate. Environ Res. 104:402–9.
8-Lipsett M, Hurley S, Ostro B. 1997. Air pollution and emergency room visits for asthma in Santa Clara County, California. Environ Health Perspect. 105:216–22.
9-Barnett AG, Williams GM, Schwartz J, Neller AH, Best TL, Petroeschevsky AL, 2005.Simpson RW. Air pollution and child respiratory health: a case-crossover study in Australia and New Zealand. Am J Respir Crit Care Med. 171:1272–8.
10-Villeneuve PJ, Chen L, Rowe BH, Coates F. 2007.Outdoor air pollution and emergency department visits for asthma among children and adults: a case-crossover study in northern Alberta, Canada. Environ Health. 6:40.
11-Stieb DM, Burnett RT, Beveridge RC, Brook JR. 1996. Association between ozone and asthma emergency department visits in Saint John, New Brunswick, Canada. Environ Health Perspect. 104:1354–60.
12-Tecer LH, Alagha O, Karaca F, Tuncel G, Eldes N. 2008. Particulate matter (PM(2.5), PM(10–2.5), and PM(10)) and children's hospital admissions for asthma and respiratory diseases: a bidirectional case-crossover study. J Toxicol Environ Health A. 71:512–20.
13-Yamazaki S, Shima M, Ando M, Nitta H. 2009. Modifying effect of age on the association between ambient ozone and nighttime primary care visits due to asthma attack. J Epidemiol. 19:143–51.
14-Cao J, Cheng Y, Zhao N, Song W, Jiang C, Chen R, Kan H. 2009. Diurnal temperature range is a risk factor for coronary heart disease death. J Epidemiol. 19:328–32.
15-Kyobutungi C, Grau A, Stieglbauer G, Becher H. 2005. Absolute temperature, temperature changes and stroke risk: a case-crossover study. Eur J Epidemiol. 20:693–8.
16-Souza, A.; Pavão, H. G.; Lastoria, G.; Gabas S. G.; Paranhos Filho, A. C.; Cavazzana, G. H.. 2009. Distribuição espacial da relação precipitação/número de dias de chuvas em Campo Grande-MS. In: SERHIDRO PS-2009-2 Seminário de recursos hídricos da bacia hidrográfica do Paraíba do Sul, 2009, Taubaté. SERHIDRO PS-2009-2 Seminário de Recursos Hídricos da Bacia Hidrográfica do Paraíba do Sul.
17-Souza, A; Granja, S.C. 1997. Estimativa dos parâmetros "C" e "K" do modelo de Weibull e da direção dos ventos para Campo Grande e Dourados, MS, Brasil. Revista Brasileira de Agrometeorologia, Santa Maria, v.5, n.1, p.109-114.
18- Bai et al. 2014. Temperature, hospital admissions and emergency room visits in Lhasa, Tibet: A time-series analysis. Science of The Total Environment. Volume 490, 15 August 2014, Pages 838–848. doi:10.1016/j.scitotenv.2014.05.024
19 . Chatkin JM, Zaslavsky C, Orlandini L, Zagoury EL, Scliar MJ. 1986. A inclusão da asma brônquica nos programas de controle de doenças respiratórias agudas. J Pneumol. 12(3):167-9.
20. Trippia SMG, Rosário Filho N, Ferrari FP. 1998. Aspectos clínicos da asma na criança: análise de 1009 pacientes de um ambulatório especializado. Rev Bras Alergia Imunopatol. 21(3):75-82.
21. Fischer G B. 1984. Relação entre a incidência de crises asmáticas e as alterações do clima. J Pneumol. 10 Supl 1:75.
22. Guirau LM, Solé D, Naspitz CK. 1997. Bronchoprovocation with methacholine in children under two years old: a follow-up study. J Investig Allergol Clin Immunol. 7(2): 110-4.
23. Pastorino AC, Accioly AP, Lanzellotti R, Camargo MC, Jacob CM, Grumach AS. 1998. [Asthma- clinical and epidemiological aspects of 237 outpatients in a specialized pediatric unit]. J Pediatr (Rio J). 74(1):49-58.
24. Fiore RW, Comparsi AB, Reck CL, Oliveira JK de, Pampanelli KB, Fristcher CC. 2001. Variação na prevalência de asma e atopia em um grupo de escolares de Porto Alegre, Rio Grande do Sul. J Pneumol. 27(5):237-42
25. Ferrari GF, Silva MS, Bossolan G, Borges VTM, Curi PR. 1991. Estudo retrospectivo (1980-1989) de 294 pacientes asmáticos estudados no ambulatório de pneumologia e alergia respiratória do HE/FMB-UNESP. Parte II: Características da crise, antecedentes, desencadeantes. J Pneumol. 17 Supl 1:2-3.
26. Correia AL, Macedo AG, Silva AMC, Silva COS, Botelho C. 2002. Infecção Respiratória Aguda (IRA) em crianças menores de cinco anos e períodos climáticos. Pulmão RJ. 11(4):191-6.
27. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. 1995. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 332(3):133-8.
28. Zhang L, D'Avila NEM, Santos JCD, Ferruzzi EH, Chitolina J, Costa MMG. 1999. [Tendência das hospitalizações por crises de asma em crianças em um período de dezoito anos]. J Pediatr (Rio J). 75(4):249-55.
29. Son J-Y, Bell ML, Lee J-T (2014) The impact of heat, cold, and heat waves on hospital admissions in eight cities in Korea. International journal of biometeorology: 1–11.
30. Guo Y, Jiang F, Peng L, Zhang J, Geng F, et al. (2012) The association between cold spells and pediatric outpatient visits for asthma in Shanghai, China. PloS one 7: e42232.
31. Donaldson G, Seemungal T, Jeffries D, Wedzicha J (1999) Effect of temperature on lung function and symptoms in chronic obstructive pulmonary disease. European Respiratory Journal 13: 844–849.
32. Larsson K, Tornling G, Gavhed D, Muller-Suur C, Palmberg L (1998) Inhalation of cold air increases the number of inflammatory cells in the lungs in healthy subjects. European Respiratory Journal 12: 825–830.
33. Mäkinen TM, Juvonen R, Jokelainen J, Harju TH, Peitso A, et al. (2009) Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respiratory medicine 103: 456–462.
34. Basu R, Samet JM (2002) Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiologic reviews 24: 190–202.
35. Hajat S, Haines A (2002) Associations of cold temperatures with GP consultations for respiratory and cardiovascular disease amongst the elderly in London. International Journal of Epidemiology 31: 825–830.
36. Goodman PG, Dockery DW, Clancy L (2004) Cause-specific mortality and the extended effects of particulate pollution and temperature exposure. Environmental health perspectives 112: 179.
37. Yang J, Ou C-Q, Ding Y, Zhou Y-X, Chen P-Y (2012) Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environmental Health 11: 1–9.
38. Guo Y, Punnasiri K, Tong S (2012) Effects of temperature on mortality in Chiang Mai city, Thailand: a time series study. Environ Health 11: 36.
39. Xu Z, Huang C, Hu W, Turner LR, Su H, et al. (2013) Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occupational and Environmental Medicine 70: 730–735.
40. Buckley JP, Richardson DB (2012) Seasonal modification of the association between temperature and adult emergency department visits for asthma: a case-crossover study. Environmental Health 11: 1–6.
41. Anderson GB, Bell ML (2011) Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environmental health perspectives 119: 210.
42. Michelozzi P, De Sario M, Accetta G, de'Donato F, Kirchmayer U, et al. (2006) Temperature and summer mortality: geographical and temporal variations in four Italian cities. Journal of epidemiology and community health 60: 417–423.
43. Gasparrini A, Armstrong B, Kenward M (2010) Distributed lag non-linear models. Statistics in medicine 29: 2224–2234.
44. Gasparrini A (2011) Distributed lag linear and non-linear models in R: the package dlnm. Journal of Statistical Software 43: 1.
45. Almqvist C, Worm M, Leynaert Bnd (2008) Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy 63: 47–57. [PubMed]
46. Xu Z, Huang C, Su H, Turner LR, Qiao Z, et al. (2013) Diurnal temperature range and childhood asthma: a time-series study. Environ Health 12: 12.
1. Federal University of Mato Grosso do Sul, Institute of Physics, Campo Grande, MS, Brazil. E mail : amaury.de@uol.com.br
2. Federal University of Mato Grosso, Campus Rondonopolis, Rondonopolis, MT, Brazil