

Vol. 38 (Nº 58) Year 2017. Page 23
Elena TARASOVA 1; Tatiana KOCHEGURA 2; Natalya ALEXANDRUSHKINA 3; Lyalya GABBASOVA 4; Zhanna AKOPYAN 5
Received: 03/08/2017 • Approved: 01/09/2017
ABSTRACT: Societal challenges create significant risks for society, economies, and public administration systems. In response to these challenges, the rapid development of medical science has made a significant contribution to improving the health of the population. This review analyzes the main trends in EU health research development and shows how the introduction of innovative approaches and new technologies (personalised medicine, electronic and mobile health) contributes to the well-being of the population while combatting the consequences of demographic changes. |
RESUMEN: Los desafíos sociales crean riesgos significativos para la sociedad, las economías y los sistemas de administración pública. En respuesta a estos desafíos, el rápido desarrollo de la ciencia médica ha contribuido significativamente a mejorar la salud de la población. Esta revisión analiza las principales tendencias en el desarrollo de la investigación en salud de la UE y muestra cómo la introducción de enfoques innovadores y nuevas tecnologías (medicina personalizada, salud electrónica y móvil) contribuye al bienestar de la población mientras la lucha contra las consecuencias de los cambios demográficos. |
Priority directions and trends in the scientific and technological development of the EU are determined by the European Commission and implemented through EU Framework Programs (FP). These programs are the main mechanism for supporting research and development in the EU. Financing is focused on priority areas of this research, one of which is “Health”.
Since 1984, the EU has implemented seven Framework Programs. The Seventh FP (2006-2013) played an important role in strengthening the competitiveness of the EU, increasing funding for scientific research, and implementing projects that had a significant impact on the dissemination of new knowledge, the formation of a European Research Area, the creation of new jobs, and the development of small and mid-sized businesses (Mialhe, 2012).
It is important to note that the EU not only pays attention to the development of scientific research, but also the development of research databases and related infrastructure. In Europe, for example, there are various biological banks and scientific registries that open up great opportunities for innovative joint research on the origin of risk factors for various diseases, such as dementia, cancer and cardiovascular diseases.
The EU Framework Program for research and innovation “Horizon 2020” started in January 2014. The goal of the Program is to ensure scientific research produced at international and global levels, remove barriers to innovation, and strengthen cooperation between the public and private sectors in the field of scientific development. With respect to medical research, the Program aims to reduce health care costs by increasing the availability of medical information, personalized medical care, and the creation of “smart” care systems for patients (Mialhe, 2012).
Proirities of scientific research in the health field are determined in accordance with the Europe 2020 strategy (Komaba, 2015). It is expected that EU socio-economic problems in the coming years will be associated mainly with demographic changes and the dynamics of economic development of the expanding European Union: an increase in the life expectancy of citizens and a decrease in the birth rate together with increased mobility of the population will lead to an increase in the demand for better health care systems (European Commission, 2015). In response to the objectives set out in the Strategy, the direction “Health” in the EU FP “Horizon 2020” has grown into “Health, Demographic Change and Well-Being”.
The fight against specific societal challenges and attention to certain areas of public health have determined the priorities and trends in medical technology and scientific development in the field of EU health:
- Transition to personalised medicine
- Research aimed at ensuring the well-being and quality of life of the elderly population
- Introduction of electronic and mobile health care
The main research directions were determined by an analysis of the Health Work Programs of the Seventh Framework Program of the EU and the Horizon 2020 Framework Program, the official reports of the European Commission’s Directorate General for Research and Innovation, Directorate for Health, the conclusions of expert groups, the analysis of Framework Program “Horizon 2020” projects available in the CORDIS system and the analysis of world scientific literature.
In terms of progress in the treatment of many acute and chronic diseases in the EU, medicine and public health are generally seen as not effective enough: global diseases require a proactive use of preventive measures, as well as a personalized approach to treatment. At present, socially significant non-infectious diseases including diabetes, cardiovascular and oncological diseases are usually detected at later stages and only begin treatment in severe stages of disease development. According to forecasts, over the next several years, a scenario is possible where spreading epidemics of type 2 diabetes, neurodegenerative disorders and some cancers could lead to economic catastrophe for national health systems.
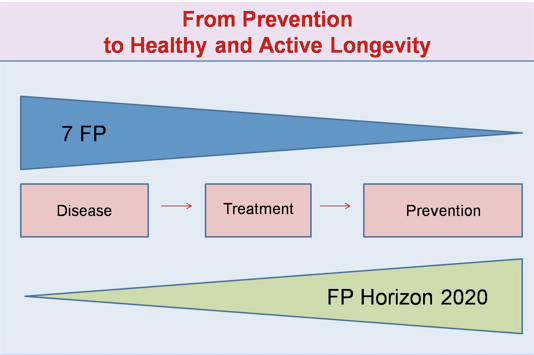
The problems facing modern health care necessitate changes in the organization of medical care for the public. A prime example of such change is the concept of predictive, preventive and personalized medicine (PPPM), which was a result of controlling the spread of diseases of different etiologies. Cost-effective disease management and the critical role of PPPM in modernizing health care have been recognized as priorities for global and regional health-related organizations, including the UN and the EU (Lemke & Golubnitschaja, 2014). In general, this paradigm shift in the area of public health can be presented graphically (Fig. 1).
Figure 1
The shift of paradigms in Healthcare in Europe.
Personalized medicine (Testori, 2011) can be described as a strategy for the prevention, diagnosis and treatment of diseases based on individual molecular genetic characteristics. The main approaches to personalized medicine include the following:
- Prediction based on genomic data of the probability of occurrence of a disease with the subsequent development of an individual prevention schemes
- Transition from a typical clinical diagnosis to a personalized diagnosis of the disease based on molecular profiling, followed by the monitoring of biomaterial throughout patient life
- Choice of therapeutic strategies, taking into account individual patient characteristics
- Personalized selection of medications and monitoring of treatment through the use of biomarkers.
Combined, these approaches should substantially reduce mortality rates from the most common socially significant non-communicable diseases, and increase the economic efficiency of the health system as a whole.
One of the most important aspects in the field of personalized medicine is the formation of groups of patients with similar “molecular features” by using biomarkers, markers that can serve as indicators of the health status of the whole individual. With the help of identified biomarkers, it will be possible to adapt medical interventions to specific patient groups instead of applying a one size fits all approach. Also, similar biomarkers (European Commission, 2015) in future will allow the “predicting” of health risks associated with the side effects of drugs in certain groups of patients, resulting in a significant decrease in the statistics on the number of follow up visits to medical facilities.
The search for characteristic biomarkers can help to identify, test and develop new treatments for rare diseases. The emphasis on the study of molecular causes and mechanisms of rare diseases is justified as there is a worldwide trend of increasing numbers of orphan diseases, related to both the improvement of diagnostic methods and the emergence of new mutations in human genes (Kontoghiorghe, Andreou, Constantinou, & Kontoghiorghes, 2014). In addition, the search for innovative approaches in the study of these diseases can contribute to understanding the development of other pathologies (Bai, et al., 2013).
European research includes studies using a personalised approach and the use of the genomic, epigenetic, metagenomic, metabolic, microbiotic and proteomic studies (‘omic’ technologies) of an individual in combination with lifestyle and environment, aimed at identifying risk factors and preventing diseases in a certain group of the population (Alyass, Turcotte, & Meyre, 2015). Through this approach, health workers will be able to identify and offer more targeted treatments, avoid medical errors and prevent side effects from taking medications.
One example illustrating the use of biomarkers for the early diagnosis of oncological pathology is the European project FORECEE (Female Cancer Prediction Using Cervical Cancer) using ‘omic’ technology for individualizing screening and prevention (Forcecee, 2017). The project is aimed at developing a diagnostic testing system that allows identifying the risks of cervical, breast and ovarian cancer development on the basis of new molecular factors, as well as bacterial and viral infections of the female sex organs.
In fact, the model of the “average patient” that has been used in health care for the development and testing of medicines, and the selection of appropriate treatment regimens has not taken into account the “molecular profile” of patients. At the same time, the “molecular profile” in combination with the ecology of the environment and lifestyle determines susceptibility to many diseases, the course of these diseases and the response of the body to ongoing treatment. Personalized medicine, in turn, is focused on a specific person and involves a transition to the prevention and/or early treatment of diseases, auxiliary treatments and medicine, and considers individual characteristics of the body (Horgan, et al., 2014).
It should be noted that the EU FP “Horizon 2020” pays much attention to screening and effective preventive measures, developed not only on the basis of medical data, but also data on the lifestyle and quality of life of the patient, taking into account gender and ethnic characteristics of different population groups.
Of increasing importance is the involvement of the patient in the treatment and diagnostic process. One more principle has been added to the fundamental principles of the PPPM concept, a “partnership” between the doctor and the patient. The new model of 4P Medicine (Predictive, Preventive, Personalized and Participatory Medicine) provides the same goals as PPPM, however patients become active participants in the preventive, therapeutic and diagnostic processes (Hood & Flores, 2012).
With the help of easy-to-use devices (“smart” watches with a built-in pedometer, heart rate sensor, and blood pressure monitor, or an “intelligent” plate that allows you to control the qualitative and quantitative composition of food), the patient can objectively assess his overall motor activity, cardiovascular system at rest and during physical exertion, as well as inaccuracies and compliance with diet, while taking medications prescribed by a doctor. This participation allows the patient to learn the skills of a healthy lifestyle and apply them in daily life, because constant adherence to the principles of health care is fundamental for the prevention of most non-infectious diseases (cardiovascular, respiratory, cancer, diabetes, neuropsychiatric disorders, and musculoskeletal system disorders) or adherence to the treatment of an already existing chronic disease. At the same time, the attending physician has the possibility of not only 24 hour monitoring, but also remote and objective assessments from regular patient reports on the current state of patient health and the work done to maintain and strengthen health.
The development of personalized medicine and its introduction into the healthcare system of EU countries is aimed at strengthening the health of all population groups, and not only with the help of the latest achievements in medicine (molecular medicine, ‘omic’ technologies, innovative diagnostic platforms, and others), but also in creating active roles for the patient in relation to providing them with individual environmental factors that determine good health.
According to the Europe 2020 strategy (European Commission, 2010) research in the field of health until 2020 should focus on issues of the aging population. In the near future, large demographic changes are expected in Europe: The number of Europeans over the age of 65 is projected to almost double (from 85 million in 2008 to 151 million by 2060), and the number of older people over 80 will increase threefold over the same period (from 22 to 61 million people) (Lemke & Golubnitschaja, 2014).
It should be noted that many diseases that are characteristic of older people can begin as at a young age. Obesity, diabetes mellitus, mental disorders and neurodegenerative diseases, susceptibility to various infectious diseases, musculoskeletal disorders, sensory disorders, non-treatable rare diseases, cancer and cardiovascular diseases are now the main medical problems and will undoubtedly, pose a threat to public health in the future.
All these factors dictate the need to search for innovative methods to improve the quality of life and increase the life expectancy of the aging population, diagnose and treat age-associated diseases, introduce new innovative technologies based on information systems, and develop new products aimed at maintaining the well-being of elderly people.
The increase in the life expectancy of Europeans demonstrates the success of existing health care systems; however, this success also necessitates questioning the quality of life of elderly people (n.a., 2011). Chronic diseases require long-term or constant care by relatives for elderly patients, accruing financial costs, and for the health care system, chronic diseases generate increasing demands and costs for providing appropriate treatment and care (Lemke & Golubnitschaja, 2014).
To maintain the high quality of medical care, it is necessary to change the current paradigm and reorient the activities of doctors, managers, and health care organizers primarily to health promotion, disease prevention and early diagnosis.
It is expected that a new perspective on health, through the lens of demographic change, will prevent, detect and treat diseases, enable older people to remain active with control over their own health, while increasing understanding of the causes and mechanisms underlying longevity, healthy aging and diseases associated with age.
An example of a European project aimed at maintaining the healthy and active longevity of the elderly is the ELF@Home project (Elderly self-care based on self-check of health conditions and self-fitness at home) (n.a., 2017). The main innovative feature of the ELF@Home project is the development of a fitness platform for the elderly, which is easy for home use. An elderly person is in their own house, while using a special device, the platform captures their movements during the day and transfers the data to a mini-computer which performs an analysis of motor activity. The results of pulse and blood pressure measurements from the wireless pulse oximeter and the tonometer are also sent to the computer. The home TV serves as a monitor and user interface for this system. On the basis of the received data on physical activity and medical indicators, ELF@Home creates an individual fitness plan, checks health indicators before and after exercise, and generates a health status report. The individual has the opportunity to interact with the application with the aid of gestures or voice. In this way, ELF@Home supports active and healthy longevity at home and helps aged people to live independently.
Active and healthy longevity, an increase in life expectancy and working age will contribute to the emergence of new jobs, new markets, and the development of the services and industrial sectors. In response to these challenges, a new concept is being initiated in the EU, the “Silver Economy”. A precise definition of the silver economy has not yet been formulated, however, it is primarily associated with new economic opportunities that are rising as a result of the change in demands of the population older than 50 years. The silver economy is aimed at improving the quality of life of elderly people and their inclusion in public life and economic activity. It is expected that by 2020 the purchasing power of the older generation (60+) will reach USD15 trillion (Eatcock, 2015).
The new direction of EU FP “Horizon 2020” is the close interaction of medicine, and information and communication technologies, which has led to the emergence of eHealth. Medical ICTs are designed to develop new platforms and technological solutions that are capable of timely and effective solutions in an ever changing and growing information society.
The use of ICT provides substantial support to modern healthcare in the creation of innovative diagnostic tools (Gschwind, 2015), monitoring of patient health status (in inpatient and outpatient settings, as well as self-management devices for managing their own health), self-maintenance devices and self-observation of the elderly, rehabilitation, and counseling (Fardoun & Mashat, 2017).
EHealth in the EU Framework Program Horizon 2020 implies the active use of ICT solutions and services in health care to track internal and external factors that affect public health and the health system as a whole.
Digital personalized models and tools for individual clinical tasks are already available, however, there is a need for closer integration of patient information, for example, using multi-scale, multilevel physiological models of the patient's current condition, and specific population and data for the generation of new clinical information with the aim of managing the health of patients. Here, in vivo and in vitro data on the patient, genomic and epigenetic research results, and data on the nature of nutrition and home environment are also applicable. It is assumed that this kind of integrated digital representation of comprehensive information about the patient (the “digital patient”) will make it possible to maximize use of all information about the patient and to develop optimal treatment strategies to preserve health (Saner & van der Velde, 2016). At the same time, much attention to the “digital literacy” of the patients themselves, their training in working with electronic services for a healthy lifestyle and good health, will be required.
An example of the development of such technologies is the European project named PD_Manager (mHealth platform for Parkinson's disease) (n.a., 2017). The project aims to create innovative mobile devices for managing the ecosystem of a patient suffering from Parkinson's disease. With the help of light, inconspicuous, built-in mobile devices, sensors (sensory insoles, smart clocks, electronic containers for tablets, bracelet) information about motor symptoms of the disease (tremor, bradykinesia, and gait disturbance), and non-motor symptoms (sleep, speech, and cognitive frustration), will arrive on a smartphone with a set of relevant applications. The information obtained this way will allow for timely changes in the drug therapy of a particular patient; also, it will also allow for following the adherence of medical recommendations to patients, which is key to prolonging and improving the quality of life, including a reduction in the number of falls. With advances in ICT, patients will be encouraged and motivated to follow treatments, comply with dietary recommendations, and independently perform physiotherapy procedures to maintain their condition.
Scientific research in the field of Health Research in the EU FP Horizon 2020, in contrast to the Seventh EU FP, is more focused not on fundamental, but on applied biomedical research, in particular, on the development of new methods of treatment with clinically proven efficacy, taking into account age characteristics, gender differences and comorbid pathology.
Analysis of the priority research topics in the field of Health Research has shown that a new model of medicine is beginning to be implemented in Europe, characterized by the transition from the disease-treatment approach to the prevention and early diagnosis of diseases involving the patient in the preventive, therapeutic and diagnostic processes. The involvement of the patient becomes possible thanks to the use of ICT, and by increasing the “digital literacy” of the patients themselves.
The system of support for scientific research and organization of EU health is focused on combating societal challenges, primarily with demographic changes. Scientific achievements and innovative developments are designed to improve the health of the population and prolong its active longevity, which will contribute to increasing the competitiveness of the European economy.
Patients, becoming active participants in the diagnostic and treatment processes, ask relevant and informed questions based on the results of research activities. This is facilitated by the development of a more knowledgeable population and the development of technical culture for patients.
The long-term strategy for conducting research in the field of health in the EU is to find new approaches to solving the main societal challenges, which systematically allows the formation of new research topics within the EU FP “Horizon 2020” (Norstedt, 2014). Long-term planning, regular updating of priority scientific topics and the introduction of advanced technologies facilitate changing the role of science and technology in the development of society and the economy, improving the quality of life of the population and providing readiness for existing and emerging societal challenges.
The paper was carried out within the framework of the Subsidy Agreement No. 14.601.21.0004 as of December 12, 2014, RFMEFI60114X0004.
Alyass, A., Turcotte, M., & Meyre, D. (2015). From big data analysis to personalized medicine for all: challenges and opportunities. BMC Med Genomics, 8.
Bai, J. P., Barett, J. S., Burckart, G. J., Meibohm, B., Sachs, H. C., & Yao, L. (2013). Strategic Biomarkers for Drug Development in Treating Rare Diseases and Diseases in Neonates and Infants. The AAPS Journal, 447-454.
Eatcock, D. (2015, July 1). he silver economy. Opportunities from ageing. European Parliamentary Research Service. Retrieved from europarl.europa.eu: http://www.europarl.europa.eu/EPRS/EPRS-Briefing-565872-The-silver-economy-FINAL.pdf
European Commission. (2010, March 3). EUROPE 2020 - A strategy for smart, sustainable and inclusive growth (Annex 1 – Europe 2020: an Overview). Retrieved from EUR-Lex: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2010:2020:FIN:EN:PDF
European Commission. (2015). Horizon 2020 Work Programme 2016 - 2017. Health, demographic change and well-being. n.a.: European Commission Decision C (2015)6776 of 13 October 2015.
Fardoun, H. M., & Mashat, A. S. (2017). Technologies Solutions Schemes for Patients' Rehabilitation. Methodologies, Models and Algorithms. Methods of Information in Medicine, 83-87.
Forcecee. (2017, April 4). The FORECEE project. Retrieved from forecee.eu: http://forecee.eu/
Gschwind, Y. J. (2015). ICT-based system to predict and prevent falls (iStoppFalls): results from an international multicenter randomized controlled trial. European Review of Aging and Physical Activity, 12.
Hood, L., & Flores, M. (2012). A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. New Biotechnology, 613-624.
Horgan, D., Jansen, M., Leyens, L., Lal, J. A., Sudbrak, R., & Hackenitz, E. (2014). An Index of Barriers for the Implementation of Personalised Medicine and Pharmacogenomics in Europe. Public Health Genomics, 287-298.
Komaba, Y. (2015). European Union’s Growth Strategy for Healthcare. Fujitsu Scientific and Technological Journal, 90-96.
Kontoghiorghe, C. N., Andreou, N., Constantinou, K., & Kontoghiorghes, G. J. (2014). World health dilemmas: Orphan and rare diseases, orphan drugs and orphan patients. World Journal of Methodology, 163.
Lemke, H. U., & Golubnitschaja, O. (2014). Towards personal health care with model-guided medicine: long-term PPPM-related strategies and realisation opportunities within ‘Horizon 2020’. The EPMA Journal, 8.
Mialhe, A. (2012). Profiles, motivations and expectations of participants to EC funded research in Health (2002–2010): A statistical analysis. IRBM, 202-210.
n.a. (2011). Economist Intelligence Unit. The future of healthcare in Europe. London: The Economist Intelligence Unit Limited.
n.a. (2017, April 4). The ELF@Home Project,Elderly self-care based on self-check of health conditions and self-fitness at home. Retrieved from elfathome: http://www.elfathome.eu/
n.a. (2017, April 4). The PD_manager project. Retrieved from parkinson-manager: http://www.parkinson-manager.eu/
Norstedt, I. (2014). Horizon 2020: European perspectives in healthcare sciences and implementation. The EPMA Journal, A1-A10.
Saner, H., & van der Velde, E. (2016). eHealth in cardiovascular medicine: A clinical update. European Journal of Preventive Cardiology, 23.
Testori, C. P. (2011). A European view on the future of personalised medicine in the EU. European Journal of Public Health, 6-7.
1. Department of Educational and Scientific Program Coordination, Medical Research and Education Center, Lomonosov Moscow State University, Moscow, Russia, lenaronet@mail.ru
2. Department of Educational and Scientific Program Coordination, Medical Research and Education Center, Lomonosov Moscow State University, Moscow, Russia
3. Department of Educational and Scientific Program Coordination, Medical Research and Education Center, Lomonosov Moscow State University, Moscow, Russia
4. Department of Multidisciplinary Clinical Education, Faculty of Basic Medicine, Lomonosov Moscow State University, Moscow, Russia
5. Department of Multidisciplinary Clinical Education, Faculty of Basic Medicine, Lomonosov Moscow State University, Moscow, Russia